Nutrients that impact diabetic markers
Summary
Carbohydrates are made up of sugars, starch, and dietary fiber. While sugars are quickly absorbed into the bloodstream, raising blood glucose levels, dietary fiber, especially soluble fiber, slows the absorption process, making the glucose response more gradual and sustained.
Foods high in fat and protein lead to a delayed and prolonged increase in blood glucose levels, typically occurring 2 to 6 hours after the meal intake. This effect is stronger when high-fat and high-protein foods are eaten together. The increased glucose levels after a high-fat meal can lead to a higher insulin requirement compared to meals with the same carbohydrate content but lower fat content.
Micronutrients like magnesium and chromium may help improve insulin sensitivity, while magnesium deficiency can predispose or worsen type 2 diabetes.
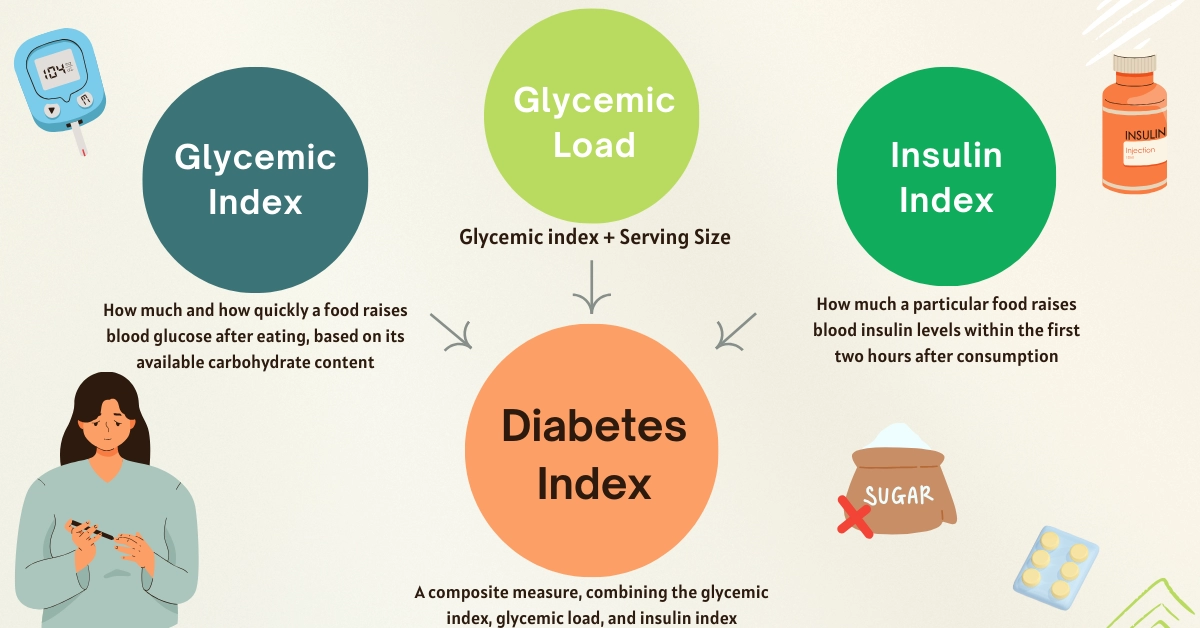
Important values that help understand the effect of the food on diabetic markers are the glycemic index, the glycemic load, the insulin index, and the newly formulated diabetes index.
The glycemic index is used to measure how much and how quickly a carbohydrate-containing food raises blood glucose levels, while the glycemic load also takes serving size into account. The insulin index is measured in a similar way, only focusing on the blood insulin level.
The diabetes index is a new value created by joining the glycemic index, load, and insulin index values. It is calculated by the following formula: DI = (GI × 0,4) + (0,3 × (GL × 5)) + (II × 0,3). A high diabetes index shows that the given food can raise blood glucose and insulin levels even in small serving sizes.
Introduction
While most people with diabetes understand the importance of avoiding high-sugar foods, sugar is not the only nutrient that affects blood sugar and insulin levels. In this article, we will discuss how all nutrients found in food can impact key diabetic markers, such as blood glucose and insulin.
Once consumed, food travels through the digestive system, where sugars and starches are broken down into glucose and absorbed primarily in the small intestine. This leads to a rise in blood glucose. However, the presence of fats, proteins, fiber, and certain micronutrients can alter both the speed and extent of glucose absorption, thereby influencing the body’s glycemic and insulin responses.
Macronutrients and Diabetes
Carbohydrates and Diabetes
Unsurprisingly, carbohydrates play the largest role in regulating blood glucose levels; however, not just the amount, but also the type of carbohydrate, makes all the difference.
The carbohydrates found in food are made up of sugars, starch, or dietary fiber. While sugars are quickly absorbed into the bloodstream, raising blood glucose levels, dietary fiber, especially soluble fiber, slows the absorption process, making the glucose response more gradual and sustained.
Most starch is broken down into sugars before it is absorbed into the bloodstream. Some starch, known as resistant starch, is similar to dietary fiber and is not absorbed; instead, it passes through the intestines. These resistant starches are fermented in the colon and can lead to bloating.
There are also short-chain carbohydrates known as FODMAPs, which are poorly absorbed in the small intestines and instead fermented by gut bacteria in the colon. FODMAP stands for fermentable, oligosaccharides, disaccharides, monosaccharides, and polyols. These carbohydrates have been researched to be associated with lower body fat and improved insulin sensitivity (1).
High sugar intake has been researched to lead to an increased chance of developing diabetes and high BMI, while high dietary fiber intake is associated with improved diabetic markers (2, 3).
The American Diabetes Association recommends eating carbohydrate sources that are minimally processed and high in dietary fiber and other nutrients (4).
The WHO strongly recommends an intake of at least 25g of dietary fiber daily, while this number is 35g according to the European Association for the Study of Diabetes (5, 6)
People with diabetes or at risk of developing it are also advised to cut out sweetened beverages and replace them with water or low-carbohydrate drinks (4).
The high intake of sugars does not cause diabetes directly, but leads to obesity, which in turn significantly increases the risk of developing type 2 diabetes.
Artificial sweeteners, also known as non-nutritive sweeteners, provide a sweet taste while adding no or few calories and not raising blood glucose levels. Some examples include aspartame (Nutrasweet), saccharin (Sweet' N Low), sucralose (Splenda), and stevia. These additives are several hundred times sweeter than sugar, so small amounts are needed to achieve the desired taste. That being said, they should be used in moderation and with caution, as more research is necessary to understand their general impact on health (7).
Thus, overall, the recommendations regarding carbohydrates are not surprising: to eat more high-fiber and low-sugar fruits and vegetables, and less processed and refined sugars.
Fats and Proteins
Foods high in fat and protein lead to a delayed and prolonged increase in blood glucose levels, typically occurring 2 to 6 hours after the meal intake. This effect is stronger when high-fat and high-protein foods are eaten together (8).
The increased glucose levels after a high-fat meal can lead to a higher insulin requirement compared to meals with the same carbohydrate content but lower fat content (9).
The reasons for this delayed glucose response are not entirely understood. Fats cause the stomach to empty later and may lead to increased glucose production in the liver, as well as lowered insulin sensitivity (10).
Protein can cause elevated glucagon secretion, which is a hormone responsible for increasing blood glucose levels. Glucose can also be synthesised from protein in a process called gluconeogenesis (10).
Micronutrients and Diabetes
Some vitamins have been researched to improve diabetic markers through various mechanisms.
Most people with diabetes have a magnesium deficiency. This may be due to a decreased intake resulting from a restricted or unhealthy diet, or to increased loss through urine, often associated with high blood insulin and glucose levels.
Among other functions, magnesium plays a role in insulin metabolism and cellular glucose uptake. A magnesium deficiency may predispose or worsen type 2 diabetes (11). Thus, magnesium supplements may improve insulin resistance and reduce oxidative stress.
Similarly, chromium is a trace element, commonly found in vegetables, legumes, and whole grains, which can help improve insulin sensitivity and glucose control (12).
Prolonged vitamin C supplementation can reduce blood glucose levels after meals and act as a helping agent in diabetes treatment (13).
Other micronutrients that play a role in regulating glucose and insulin balance in the body include zinc, vitamin D, vitamin K, B-complex vitamins, selenium, and others (14, 15, 16, 17).
Glycemic Index and Load
The glycemic index (GI) is a tool used to assess how carbohydrate-containing foods affect blood sugar levels. It measures how much and how quickly a food raises blood glucose after eating, based on its available carbohydrate content.
GI values range from 0 to 100, with pure glucose assigned a value of 100, and foods that contain no carbohydrates scoring 0.
However, the glycemic index is affected not only by carbohydrates but also in part by fats and protein.
On our website, we have gathered a comprehensive list of the glycemic index values of over 600 foods.
The glycemic load (GL) is closely related to the glycemic index, but it goes a step further by also considering the amount of available carbohydrates in a typical serving of the food.
It is calculated using the formula:
GL = (GI × available carbohydrates in grams per serving) ÷ 100
While the GI reflects the quality of carbohydrates by measuring how quickly they raise blood sugar, the GL also accounts for the quantity consumed.
Insulin Index
The insulin index (II) reflects how much a particular food raises blood insulin levels within the first two hours after consumption. It is determined by comparing the insulin response to a test food with that of a reference food, both providing the same amount of energy, typically 250 calories or 1000 kJ.
While the glycemic index is a well-researched indicator of how foods influence blood glucose, it has limitations, especially for foods low in carbohydrates, such as lean meats, some vegetables, and dairy products. In such cases, the insulin index serves as a more informative measure of the body’s metabolic response.
If interested, you can find a more in-depth comparison between the glycemic and insulin indices.
The Diabetes Index
Taking into account the glycemic response, the insulin response, and the serving size of foods, we have created a new value called the diabetes index. This value is a composite measure, not derived from new research, but rather calculated based on existing values, combining the glycemic index, glycemic load, and insulin index.
The diabetes index is calculated by the following formula:
DI = (GI × 0,4) + (0,3 × (GL × 5)) + (II × 0,3)
In this formula, the glycemic index contributes 40% to the overall diabetes index value, while the glycemic load and insulin index values each contribute 30%.
The glycemic load value is multiplied by 5 to bring its value closer to and match the scale of the average glycemic or insulin index values. In this way, we put all three components on a similar numerical scale, ensuring none is disproportionately underrepresented.
For example, papaya has a glycemic index of 38, a glycemic load of 5, and an insulin index of 129, resulting in a diabetes index of 61.
DI of papaya = (38×0,4) + ((5×5)×0,3) + (129×0,3) = 61
A low diabetes index means that a food is more likely to cause a lower rise in blood glucose and insulin levels.
Sources.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10745595/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10384374/
- https://pubmed.ncbi.nlm.nih.gov/10805824/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10725816/
- https://www.who.int/publications/i/item/9789240073593
- https://pubmed.ncbi.nlm.nih.gov/37069434/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11233937/
- https://www.researchgate.net/publication/353587710
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3609492/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3836096
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4549665/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10652672/
- https://dom-pubs.onlinelibrary.wiley.com/doi/abs/10.1111/dom.13571
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4573932/
- https://www.sciencedirect.com/science/article/pii/S2666149723000555
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9671203/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10075028/
