Calcium — Food Sources, Health Benefits & Deficiency Symptoms
Introduction
Calcium is an essential mineral fundamental to our normal physiological functioning. It is essential for maintaining overall health.
We often think that calcium is required for healthy bones and teeth; however, calcium has numerous other vital functions besides maintaining bone and teeth structure.
Table of contents
- Physiological and Biochemical Functions of Calcium
- Nutrition and Food Sources
- The Daily Requirement of Calcium
- Foods Rich in Calcium
- Health Impact
- Calcium Levels
- Calcium Deficiency
- Hypercalcemia
- Calcium and Oxalates
- Coffee, Calcium, and Osteoporosis
- People Who Should Focus on Calcium Intake
- Ca:P, Ratio Between Calcium and Phosphorus
- Calcium Supplementation
- References
Physiological and Biochemical Functions of Calcium
The main factors regulating calcium levels in the body are the parathyroid hormone (PTH) synthesized by the parathyroid glands, calcitonin made by the “C” cells of the thyroid gland, and vitamin D (calcitriol).
Parathyroid hormone acts on the kidneys, bones, and digestive system to increase blood calcium levels. PTH also stimulates calcitriol formation in the kidneys, which targets the small intestines to increase calcium absorption. Calcitonin, on the other hand, decreases calcium absorption in the intestines and kidneys, lowering blood calcium levels.
In healthy people, the parathyroid hormone regulates and monitors serum calcium levels and prevents abnormal calcium level changes via calcium-sensing receptors.
Calcium is used in numerous biochemical reactions, such as muscle contraction, nerve signal transmissions, heart contraction, and enzymatic and hormone secretory functions.
An essential aspect of calcium functionality is the constriction (tightening) and dilatation of blood vessels. The arterial system is lined with smooth muscles, which constrict or dilate due to the changes in cells’ calcium levels regulated by our nervous system. This process is one of the mechanisms of blood pressure regulation, and medications called calcium channel blockers target this process (1, 2).
Nutrition and Food Sources
In this section, we will discuss the daily requirements and main food sources of calcium and different nutritional habits that might affect the absorption and usage of calcium.
The Daily Requirement of Calcium
The daily requirement of calcium depends on age, gender, and if there is pregnancy or lactation.
This table indicates the recommended dietary allowance (RDA) (3).
| Age | Male | Female | Pregnant | Lactating |
| 0–6 months* | 200 mg | 200 mg | ||
| 7–12 months* | 260 mg | 260 mg | ||
| 1–3 years | 700 mg | 700 mg | ||
| 4–8 years | 1,000 mg | 1,000 mg | ||
| 9–13 years | 1,300 mg | 1,300 mg | ||
| 14–18 years | 1,300 mg | 1,300 mg | ||
| 19–50 years | 1,000 mg | 1,000 mg | 1,000 mg | 1,000 mg |
| 51–70 years | 1,000 mg | 1,200 mg | ||
| >70+ years | 1,200 mg | 1,200 mg
|
The RDA of calcium increases after the age of 50. As we grow older, due to normal aging processes, we risk having brittle and weaker bones at risk of fracture; thus, supplementing with calcium can help decrease the risk (3).
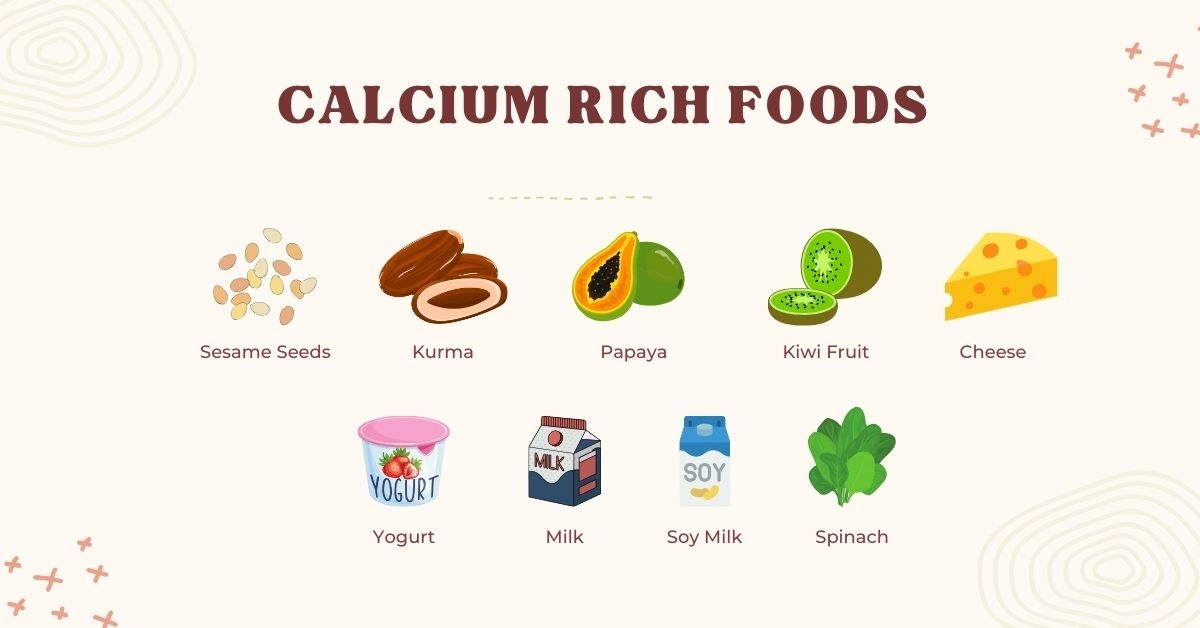
Foods Rich in Calcium
Dairy products are one of the richest sources of calcium. However, several other foods are also good sources of calcium.
Below is a table indicating the calcium content of foods per 100g in milligrams.
| Food | Calcium Content |
| Cheddar cheese | 710mg |
| Gouda | 700mg |
| Milk | 125 mg |
| Yogurt | 110mg |
| Tofu | 683mg |
| Soy milk | 25mg |
| Sardines | 382mg |
| Goat Cheese | 298mg |
| Caviar | 275mg |
| Almonds | 269mg |
| Walnuts | 98mg |
| Kale | 72mg |
| Spinach | 136mg |
For individuals who don’t follow a restrictive diet, such as the vegan diet, it is easy to acquire the daily calcium requirements. However, in the vegan diet, you can also get calcium from different sources, such as tofu, leafy greens, and nuts. However, you need to eat more to satisfy your daily requirements.
Some foods, such as milk, orange juice, and cereals, are calcium-fortified, meaning they contain artificially added calcium.
Health Impact
This section will discuss how calcium impacts our health positively and negatively. In addition, we will discuss and deep dive into what we can do to keep our calcium levels normal.
Calcium Levels
Calcium levels are normal between 8.6 - 10.3 mg/dL. As mentioned above, vitamin D, calcitonin, and parathyroid hormone control our body's calcium levels.
Below, we will discuss calcium changes in the body, their causes, and symptoms.
Calcium Deficiency
We have hypocalcemia when calcium levels in the blood are <8.3 mg/dL.
One of the leading causes of low calcium levels (hypocalcemia) is thyroidectomy (removal of the thyroid). One or several parathyroid glands may be removed during thyroidectomy due to various reasons leading to decreased PTH levels (hypoparathyroidism), the primary regulator of calcium metabolism.
Less common and rare causes of hypoparathyroidism and subsequent calcium deficiency include congenital hypoparathyroidism, autoimmune disorders, genetic abnormalities, destruction of the parathyroids, PTH resistance, heavy metal or metastatic infiltration, etc. Increased or decreased magnesium levels may also impair the secretion of parathyroid hormone (4, 5, 6).
Among other causes of hypocalcemia are vitamin D deficiency, malabsorption (celiac disease, Crohn’s disease, short bowel syndrome, chronic pancreatitis, etc.), end-stage liver disease, diets rich in soluble oxalates, phosphate infusion, kidney failure, Fanconi syndrome, acute pancreatitis, sepsis, and medications such as corticosteroids or high-dose intravenous bisphosphonates (5, 6).
Usually, when there is an acute onset of hypocalcemia, it is not from dietary restriction.
Calcium and Medications
Bisphosphonates are used to treat various bone diseases; they act to reduce bone resorption. Hypocalcemia is more likely to happen during high-dose administration of the drug or if the individual has underlying vitamin D deficiency, malabsorption, unrecognized hypoparathyroidism, or impaired kidney function.
Corticosteroids lower calcium levels by reducing intestinal calcium absorption and impairing vitamin D metabolism.
Other medications associated with hypocalcemia are denosumab, cinacalcet, several chemotherapeutic drugs, and foscarnet (7, 8).
It is best to inform your doctor if you are supplementing with calcium in case he is prescribing medications.
Hypocalcemia Symptoms
Low blood calcium levels, or hypocalcemia, can be from asymptomatic at mild deficiency to life-threatening symptoms in severe cases (9). Acute hypocalcemia can result in severe symptoms requiring hospitalization, whereas chronic hypocalcemia is more likely to be asymptomatic.
The common symptoms of hypocalcemia are muscle twitching, numbness, spasms, tingling, paresthesias around the mouth or in the extremities, cramps, seizures, and, less frequently, anxiety, depression, or irritability (9, 10, 11).
During an ECG, we can also see prolonged QT intervals, which can lead to a type of arrhythmia called ventricular tachycardia (10). ECG changes mimicking heart infarction or failure can also be seen (11). Symptoms of arrhythmias include heart palpitations, lightheadedness, chest pain, and fainting or near-fainting episodes.
A rapid ionized calcium decline may cause tetany, a disorder characterized by involuntary muscle spasms or twitching in the extremities, hand and wrist muscle spasms, facial muscle spasms appearing by tapping the facial nerve, and difficulty speaking and swallowing due to throat muscle spasms (9, 10, 11).
In adults nowadays, calcinosis tetany is not due to dietary restrictions. It is due to underlying metabolic problems related to calcium metabolism. However, we can find calcinosis tetany in newborns fed cow’s milk instead of formula or breastfeeding (12).
Hypercalcemia
We have hypercalcemia when calcium levels in the blood are >10.3mg/dL.
The leading causes of hypercalcemia are cancers and hyperparathyroidism, but not dietary intake (13).
Excess of the hormone may be due to adenoma and hyperplasia of the parathyroid glands, familial hypocalciuric hypercalcemia, multiple endocrine neoplasia syndrome types 1 and 2A, various cancers (kidney cancer, leukemias, lymphomas, and rhabdomyosarcoma), hypervitaminosis D, thyrotoxicosis, acute or chronic kidney disease, the use of thiazide diuretics or lithium (14).
Let’s discuss some of the causes. Familial hypocalciuric hypercalcemia is a genetic disorder associated with an inactivating mutation in the calcium-sensing receptor gene. Hypervitaminosis D is increased vitamin D levels in the body, which can be of unknown origin, secondary to excessive milk intake, or related to conditions like sarcoidosis, tuberculosis, or fungal infections (14).
Thiazide diuretics block the thiazide-sensitive NaCl transporter and can decrease calcium excretion from the kidneys, potentially leading to hypercalcemia (15).
Milk, Dairy, and Hypercalcemia
We are less likely to develop hypercalcemia just by eating dairy or drinking too much milk. However, we might get bloated from all the lactose we are consuming. In addition, high salt intake should be considered in some cheeses.
Hypercalcemia Symptoms
High levels of calcium can cause several problems (16):
- Fatigue
- Abdominal pain
- Nausea and vomiting
- Peptic ulcers
- Constipation
- Acute pancreatitis
- Bone pain and arthritis
- Osteoporosis, osteomalacia, pathological fractures
- Kidney stones and kidney calcifications
- Excessive urination and fluid intake
- Lethargy, confusion, depression, and memory loss.
Severe hypercalcemia leads to muscle weakness and arrhythmias. On an ECG, we can see prolonged PR intervals, short QT intervals, widened QRS complex, and decreased heart rate (16).
Chronic hypercalcemia may lead to continuous bone resorption and reduced bone mineral density to the point of osteoporosis. In rare cases, severe and prolonged hypocalcemia may also be associated with osteoporosis. Osteoporosis is characterized by bone fragility and an increased risk of sudden fractures.
Calcium and Oxalates
Oxalates, or oxalic acids, are dietary factors that negatively impact calcium absorption.
During the simultaneous consumption of oxalates with calcium-rich foods and supplements, calcium ions bind to soluble oxalates, precipitate them, and reduce their absorption.
For this reason, those with calcium oxalate stones may be suggested to supplement calcium and keep a low-oxalate diet to reduce the risk of stone formation.
Coffee, Calcium, and Osteoporosis
Does coffee increase the risks of osteoporosis?
Most clinical trials indicate no or minimal link between caffeine consumption and osteoporosis.
In vitro research showed a direct effect. However, in-vivo results do not replicate the same results.
Most research that indicates a link has a selective bias because they usually indicates that the sample is female, above 40, and already on a low-calcium diet. In addition, the amount of coffee consumed is higher than the average. Thus, many biases, including selection and confounding biases, are present to conclude (17, 18, 19).
People Who Should Focus on Calcium Intake
Some of the population needs to consider calcium intake, whereas, for the majority, it is not a significant problem when they have a normal and healthy diet.
Individuals who need to pay attention to their calcium levels are postmenopausal women, people taking certain medications (mentioned above), vegans, and people with conditions like osteoporosis, advanced chronic kidney disease, hypervitaminosis D, oxalate kidney stones, and lactose intolerance.
Ca:P, Ratio Between Calcium and Phosphorus
The adequate ratio between calcium (Ca) and phosphorus (P) is 1:1 to 2:1, meaning we should consume as much or double the amount of phosphorus.
Western diets tend to have a very low Ca:P, meaning we consume much higher amounts of phosphorus than calcium, which is linked to adverse health impacts, mainly increased bone resorption. Keeping the Ca:P ratio at the correct homeostatic levels is essential for the bones and overall health (20, 21).
Calcium Supplementation
There are many available calcium supplements; the two most common are calcium carbonate and calcium citrate. Data shows that supplementing with calcium citrate is better since it has a higher absorption rate of 22-27% (22).
References
- https://www.ncbi.nlm.nih.gov/books/NBK557683/
- https://pubmed.ncbi.nlm.nih.gov/21896151/
- https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
- https://pubmed.ncbi.nlm.nih.gov/22863393/
- https://www.uptodate.com/contents/etiology-of-hypocalcemia-in-adults
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267/
- https://www.uptodate.com/contents/etiology-of-hypocalcemia-in-adults
- https://www.annemergmed.com/article/S0196-0644(95)70161-3/abstract
- https://pubmed.ncbi.nlm.nih.gov/30449546/
- https://www.ncbi.nlm.nih.gov/books/NBK430912/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279267
- https://pubmed.ncbi.nlm.nih.gov/11329115/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5045493/
- https://www.ncbi.nlm.nih.gov/books/NBK430714/
- https://pubmed.ncbi.nlm.nih.gov/22099510/
- https://www.ncbi.nlm.nih.gov/books/NBK430714/
- https://pubmed.ncbi.nlm.nih.gov/16758142/
- https://pubmed.ncbi.nlm.nih.gov/12204390/
- https://pubmed.ncbi.nlm.nih.gov/16758142/
- https://pubmed.ncbi.nlm.nih.gov/19781123/
- https://pubmed.ncbi.nlm.nih.gov/27612307/
- https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/low-calciumphosphorus-ratio-in-habitual-diets-affects-serum-parathyroid-hormone-concentration-and-calcium-metabolism-in-healthy-women-with-adequate-calcium-intake/DD7816028D839CF0E9539EC885AB99D2