Low Fodmap Diet — Fruits, Vegetables, and Snacks List for IBS
Low FODMAP Diet: Foods, Phases, Risks, & More
A low FODMAP diet has become a popular and evidence-based dietary therapy for individuals with IBS, alleviating the symptoms of bloating, abdominal distention, pain, and diarrhea. After some time, the foods are reintroduced to determine personal food sensitivities.
FODMAPs are poorly absorbed, highly fermentable, and osmotically active carbs that lead to gas and bloating in most people. FODMAPs, as such, are healthy and safe to consume, but their intake may lead to an anomalous response to FODMAP-induced physiological effects and worsen the symptoms of IBS and other functional gastrointestinal (GI) diseases (1, 2).
Understanding FODMAPs
The acronym FODMAPs stands for fermentable oligosaccharides (fructans and galactooligosaccharides), disaccharides (lactose), monosaccharides (free fructose or fructose in excess of glucose), and polyols (sorbitol, mannitol, xylitol, and maltitol).
All FODMAPs are poorly absorbed in the small intestine and rapidly fermented by colonic bacteria (gut microbiota), producing carbon dioxide, hydrogen, and/or methane gas. Their small size makes them osmotically active and attracts water into the intestinal lumen (2, 3, 4).
Fructose and polyols have a greater osmotic effect, whereas oligosaccharides (galactooligosaccharides and fructans) have greater fermentative effects (4).
Several factors are responsible for FODMAPs' poor absorption: the absence of enzymes to break down the carbohydrate bonds, the absence or reduced activity of brush border enzymes (such as lactase) in some, and the low capacity of GLUT-2 and GLUT-5 epithelial transporters (needed for fructose absorption). Additionally, molecules such as polyols are too large to get absorbed by simple diffusion (2).
Free or excess fructose (higher fructose than glucose content) is more likely to cause distention and gas, as fructose is absorbed through GLUT-5, and its absorption is enhanced in the presence of glucose through GLUT-2 (2, 4).
Animal studies demonstrate that FODMAPs may trigger IBS symptoms by other mechanisms, too: visceral hypersensitivity, increased intestinal permeability, changes in microbiota and SCFA production, and changes in motility.
Recent studies have shown that a low FODMAP diet may reduce serum levels of some proinflammatory molecules (IL-6 and IL-8), fecal bacteria (Actinobacteria, Bifidobacterium, and Faecalibacterium prausnitzii), fecal SCFAs, and n-butyric acid (3).
Low FODMAP Diet Recommendations
FODMAPs are healthy and safe, and their malabsorption is physiological, but they may trigger or worsen the gastrointestinal symptoms of individuals with sensitive GI tracts. Approximately 70-75% of individuals with IBS achieve adequate symptom relief on a low FODMAP diet.
Eliminating or restricting dietary FODMAPs will likely benefit those who see a connection between food intake and symptoms such as bloating and pain (1, 5).
A low FODMAP diet may benefit individuals with the following conditions:
- Irritable Bowel Syndrome (IBS)
- Functional bloating and abdominal distention
- Gastroesophageal reflux disease (acid reflux) with overlapping IBS
- Small intestinal bacterial overgrowth (SIBO), celiac disease, inflammatory bowel disease with overlapping IBS
- Other functional GI diseases
Individuals with troublesome diarrhea in the presence of an ileal pouch may also benefit from a low FODMAP diet (6).
The response to the diet is associated with factors like demographics, microbiome composition, metabolism, and IBS subtype (3, 7, 8).
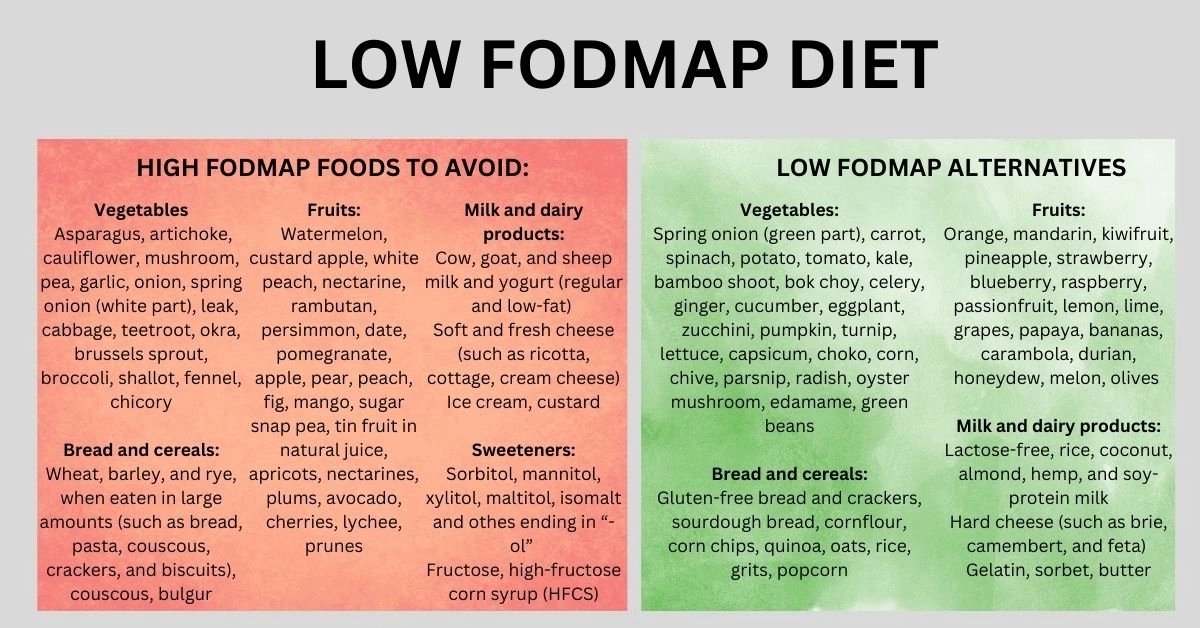
Low FODMAP Food List: Low FODMAP vs. High FODMAP
The tables below show foods divided by the type of FODMAP and their low FODMAP alternatives (1, 2, 5, 9, 10, 11).
| High FODMAP food sources | |||
| Excess fructose | Asparagus, artichoke Apple, pear, peach, watermelon, fig, mango, sugar snap pea, tin fruit in natural juice Honey sweeteners: Fructose, high-fructose corn syrup (HFCS) Drinks: Concentrated fruit sources, tropical juices, rum Large total fructose concentration: large serves of fruit, dried fruit, jam | ||
| Lactose | Cow, goat, and sheep milk and yogurt (regular and low-fat) Soft and fresh cheese (such as ricotta, cottage, cream cheese) Ice cream, custard | ||
| Fructans and/or GOS | Garlic, onion, spring onion (white part), asparagus, cabbage, leek, artichoke, beetroot, Brussels sprout, broccoli, okra, shallot, onion, pea, fennel, chicory Wheat, barley, and rye, when eaten in large amounts (such as bread, pasta, couscous, crackers, and biscuits), couscous, bulgur Legumes: Chickpeas, lentils, red kidney beans, broad beans, baked beans, soybeans, and their products (such as silken tofu) Watermelon, custard apple, white peach, nectarine, rambutan, persimmon, date, pomegranate Pistachio, cashew Soybean milk, wasabi, taro | ||
| Polyols | Cauliflower, mushroom, pea Apples, pears, apricots, nectarines, peaches, plums, avocado, cherries, lychee, prunes, watermelon Sweeteners: Sorbitol (420), mannitol (421), xylitol (967), maltitol (965), isomalt (953) and othes ending in “-ol” Artificially sweetened chewing gum and confectionery | ||
| Low FODMAP alternatives | |||
Orange, mandarin, kiwifruit, pineapple, strawberry, blueberry, raspberry, passionfruit, lemon, lime, grapes, papaya, bananas, carambola, durian, honeydew, melon, olives
| Spring onion (green part), carrot, spinach, potato, tomato, kale, bamboo shoot, bok choy, celery, ginger, cucumber, eggplant, zucchini, pumpkin, turnip, lettuce, chive, capsicum, choko, corn, parsnip, radish, oyster mushroom, edamame, canned/rinsed chickpeas. | Lactose-free, rice, coconut, almond, hemp, and soy-protein milk Hard cheese (such as brie, camembert, and feta) Gelatin, sorbet, butter, lactose-free ice cream | Snacks, bread, and cereals: Gluten-free bread and crackers, spelt products, sourdough bread, cornflour, corn chips, quinoa, oats, oatmeal, rice, grits, popcorn Garlic/onion substitutes: Garlic-infused oil |
Legumes: Green beans Nuts and seeds: | Drinks: Orange juice, coffee, sucrose-sweetened or diet soft drinks, red and white wine, gin, whiskey, vodka | Sweeteners: Sugar (sucrose), glucose, and any sweetener not ending in “-ol.” Honey Substitutes: Maple syrup, golden syrup | Fish Meat (e.g., pork, lamb, and beef) Eggs Hard Tofu, tempeh Rice noodles |
Sources of animal proteins such as meat, chicken, fish, and eggs are naturally low or absent in FODMAPs. However, processed and marinated meat may contain high-FODMAP ingredients, making the product unsuitable for individuals on a low-FODMAP diet.
Low FODMAP Diet Phases
1. Elimination or restriction
During the elimination phase, all FODMAPs are restricted or eliminated for several (4-8) weeks to determine their effect on symptoms. The diet should be discontinued if symptoms do not improve during this phase.
2. Reintroduction
After symptom improvement, patients start the reintroduction phase, during which one group of FODMAPs is added to the diet every 2-3 days, the dose is gradually increased, and the symptoms are monitored.
3. Personalization
The personalization phase allows for maintaining symptom control whilst avoiding only those FODMAPs that trigger the symptoms (4, 5, 10).
Low FODMAP Diet Downsides & Risks
Low FODMAP diet implementation is best and most effective with the help of a dietitian or GI dietitian for a more modified and individualized diet plan and decreased risk of side effects.
The main downsides and risks of a low FODMAP diet include:
- Social and lifestyle challenges: the low FODMAP diet is considered more expensive than a usual diet. It also affects some aspects of quality of life, such as social eating.
- Nutritional deficiencies: The most common is fiber deficiency due to low-carb intake. Other possible deficiencies include micronutrient deficiencies such as calcium, iron, magnesium, vitamin B1, vitamin B2, folate (vitamin B9), vitamin B12, vitamin D, and phytochemical deficiencies. To reduce the risk of nutritional deficiencies, high-FODMAP foods should be switched to nutritionally equivalent low-FODMAP alternatives, such as substituting cow’s milk with lactose-free or calcium-enriched soy protein milk. Weight loss may also occur due to a restricted diet.
- Dysbiosis (microbiota alterations): Food restrictions may decrease the intake of prebiotics (food for good bacteria), decreasing beneficial gut bacteria strains.
- Constipation due to a limited fiber intake.
- Eating Disorders: the diet may affect the emotional well-being of some individuals. Anxiety and fear about symptoms worsening and subsequent dietary restrictions may lead to the development of eating disorders, such as avoidant–restrictive food intake disorder and orthorexia nervosa.
- Limited long-term data (3, 4, 10).
Summary
A low FODMAP is an evidence-based dietary therapy for individuals with IBS; around 70-75% achieve symptom relief. FODMAPs, as such, are healthy and safe to consume, but their intake may lead to an anomalous response to FODMAP-induced physiological effects and worsen the symptoms of IBS and other functional gastrointestinal (GI) diseases.
A low FODMAP diet has 3 phases: elimination, reintroduction, and personalization, leading to maintained symptom control whilst avoiding only those FODMAPs that trigger the symptoms.
Low FODMAP diet implementation is best and most effective with the help of a dietitian or GI dietitian for a more modified and individualized diet plan and decreased risk of side effects such as nutritional deficiency, dysbiosis, constipation, and eating disorders.
References
- https://www.elsevier.es/en-revista-gastroenterologia-hepatologia-english-edition--382-articulo-the-low-fodmap-diet-for-irritable-S2444382416000213
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3966170/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5622700/
- https://www.mdpi.com/2072-6643/16/3/370
- https://gi.org/topics/low-fodmap-diet/
- https://www.medscape.com/viewarticle/716634_10
- https://onlinelibrary.wiley.com/doi/10.1111/jgh.13701
- https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.1007716/full
- https://www.uptodate.com/contents/treatment-of-irritable-bowel-syndrome-in-adults
- https://www.jnmjournal.org/journal/view.html?doi=10.5056/jnm22035
- https://www.medscape.com/viewarticle/716634_5
