Folate (Folic Acid) — Health Impact, Deficiency, and Food Sources
Introduction
Folate, also known as folic acid and vitamin B9, is a water-soluble vitamin mainly found in plant-based sources. Folic acid is commonly used to manage megaloblastic anemia and decrease the risk of neural tube defects.
Table of contents
- Absorption & Metabolism
- Physiological Role in the Organism
- Recommended Intakes
- Food Sources
- Folate Deficiency: Risk Groups & Symptoms
- Folate & Human Health
- Autism Spectrum Disorder (ASD)
- Cognitive Function & Dementia
- Depression
- Neural Tube Defects
- Preterm Birth & Congenital Disorders
- Cardiovascular Disease & Stroke
- Cancer
- Folate Toxicity & Vitamin B12 Anemia
- Folate Contraindications & Interactions
- Summary
- References
Are Folate and Folic Acid the Same?
The terms folate and folic acid are commonly used interchangeably to describe vitamin B9 or folacin, but they are not quite the same. Folate is the naturally occurring vitamin B9 from citrus fruits, leafy green vegetables, and legumes. In contrast, folic acid is the synthetic form of the vitamin used in dietary supplements and enriched or fortified foods (e.g., rice, pasta, bread, and breakfast cereals).
Folates in food are usually in the polyglutamate form due to their additional glutamate residues, whereas folic acid is in the fully oxidized monoglutamate form. Several supplementary forms of vitamin B9, such as 5-MTHF (5-methyltetrahydrofolate or methylfolate), are also monoglutamate.
Compared to folate, folic acid is more stable to heat; thus, less folic acid is lost during cooking, making it more suitable for adding to foods (1, 2, 3).
Absorption & Metabolism
After consumption, dietary folates are hydrolyzed to the monoglutamate form in the small intestines and afterward absorbed by active transport. Folic acid can also be absorbed by passive diffusion when consumed in pharmacological doses. An enzyme called dihydrofolate reductase reduces folate from monoglutamate to tetrahydrofolate (THF) form and converts it to either 5-MTHF, the predominant form in plasma, or formyl-THF.
Folate is also synthesized by large intestinal or colonic microbiota and absorbed across the colon.
Folate levels in the organism are estimated to range from 15 to 30 mg, with around 50% stored in the liver and the rest in blood and other tissues (1).
Physiological Role in the Organism
Folate is required for the synthesis of nucleic acids—DNA and RNA—and amino acid metabolism. Along with vitamin B12, it is required for the methylation of homocysteine to methionine via methionine synthase, which is metabolized to S-adenosylmethionine, and the methylation of deoxyuridylate to thymidylate in DNA formation. Impaired methylation leads to neurological problems and megaloblastic anemia (1).
We will delve more into the physiological functions of vitamin B9 below in the “Folate and Human Health” section.
Recommended Intakes
According to the 2020-2025 Dietary Guidelines for Americans, the recommended dietary allowance (RDA) for folate for adults is 400 mcg DFE (dietary folate equivalent) (4).
Below, you can see variations between ages.
| 1-3 years | 4-8 years | 9-13 years | 14 years and older |
| 150 mcg | 200 mcg | 300 mcg | 400 mcg |
The RDA increases to 500 mcg during lactation and 600 mcg during pregnancy (1, 4).
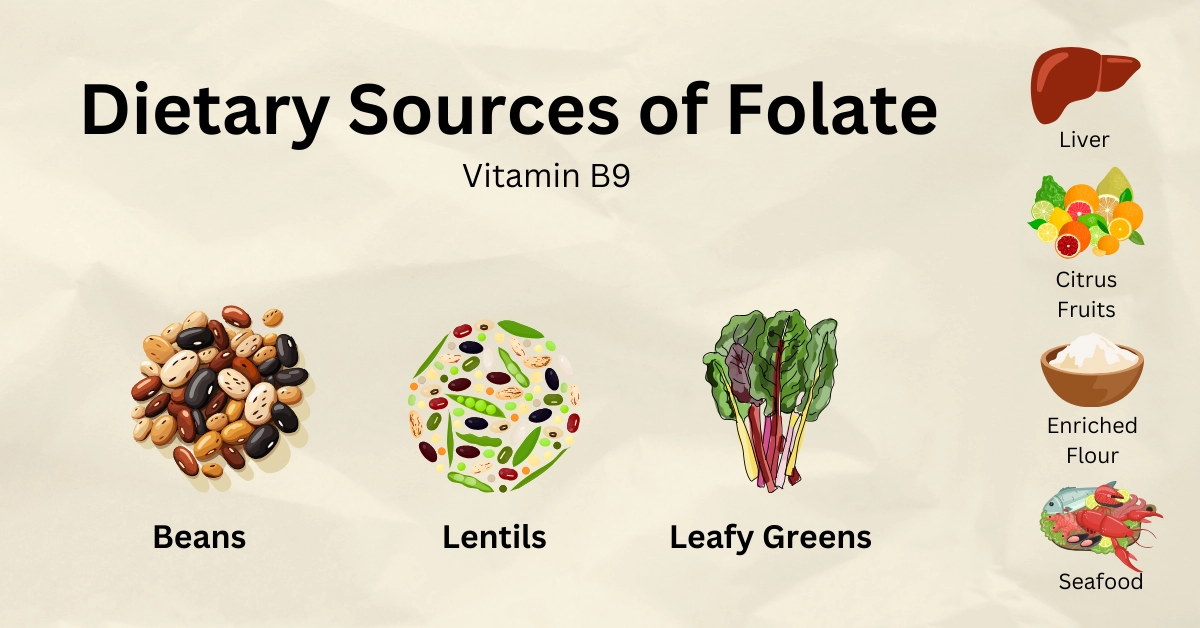
Food Sources
Folate is naturally found in vegetables, primarily dark green leafy vegetables and legumes, fruits and fruit juices, nuts, seafood, eggs, dairy products, red meat, and poultry. It can also be added to foods, as written on the packaging.
The table below shows dietary sources of vitamin B9 and its levels per serving size.
| Food Name | Vitamin B9 per Serving Size |
| Cranberry beans (cooked) | 366 mcg in 177g |
| Lentils (cooked) | 358 mcg in 198g |
| Black-eyed peas (cow peas) (cooked) | 356 mcg in 171g |
| Mung beans (boiled) | 321 mcg in 202g |
| Spinach (cooked) | 263 mcg in 180g |
| Kidney beans (cooked) | 230 mcg in 177g (1 cup) |
| Flour enriched with folic acid | 229 mcg in 125g |
| Beef liver (braised) | 215 mcg in 85g |
| Pork liver (braised) | 139 mcg in 85g (3 oz) |
| Asparagus (cooked) | 134 mcg in 90g (0.5 cup) |
| Walnuts | 98 mcg in 28.35g (1 oz) |
| Broccoli (raw) | 93.2 mcg in 148g |
| White rice (cooked) | 91.6 mcg in 158g (1 cup) |
| Orange juice | 74.4 mcg in 250g (1 cup) |
| Brussels sprouts (raw) | 53.7 mcg in 88g (1 cup) |
| Crab meat (cooked) | 43.4 mcg in 85g |
| Orange | 39.3 mcg in 130g (1 fruit) |
| Mustard greens (cooked) | 12.6 mcg in 140g |
You can visit our “Foods high in Folate” page to learn about more folate-rich leafy greens, beans, peas, and other foods.
Folate Deficiency: Risk Groups & Symptoms
Folate deficiency may result from inadequate diets, diseases affecting folate absorption or metabolism, several genetic disorders and medications, alcoholism, malignancy, pregnancy, lactation (due to an increased RDA), hemolytic anemia, and dialysis.
Folate deficiency may also result from vitamin B12 deficiency or zinc deficiency, as they are required for normal folate metabolism.
People with alcohol use disorder frequently experience nutritional deficiencies due to decreased food intake and alcohol effects on the organism. For example, alcohol reduces folate absorption and metabolism in the liver and increases its breakdown and excretion through the kidneys.
Folate malabsorption may be caused by gastrointestinal diseases, such as tropical sprue, celiac disease, Crohn’s disease, ulcerative colitis, and atrophic gastritis and gastrointestinal surgeries.
People with MTHFR genetic polymorphism 677C>T cannot convert folate to its active 5-MTHF form. This leads to less biologically active folate, elevated homocysteine levels, and an increased risk of neural tube defects and other congenital birth defects (1, 5).
Symptoms & Consequences of Folate Deficiency
Anemia
Folate deficiency causes a type of anemia called megaloblastic anemia. Anemia progresses over months without causing symptoms at early stages. Later, anemia may cause symptoms like weakness, fatigue, pale skin, lightheadedness, irritability, difficulty concentrating, chronic headaches, palpitations, cold extremities, increased heartbeat, chest pain, shortness of breath, and low blood pressure, especially after standing up. In some cases, chronic untreated anemia may result in heart failure.
Sometimes, CBC (complete blood count) tests may also show decreased neutrophil and platelet levels (5).
Elevated Serum Homocysteine
Folate deficiency, either primary or secondary to vitamin B12 deficiency, may lead to homocysteine accumulation. A mild-to-moderate increase in the amino acid homocysteine leads to atherosclerotic changes in the arteries, increasing the risk of coronary artery disease and stroke. Mild elevation is defined at 15-25 mmol/L, and moderate elevation in homocysteine levels is defined as 26-50 mmol/L (5).
Effects on Cognitive Function
Elevated homocysteine levels due to folate deficiency may lead to irritability, forgetfulness, progressive insomnia within several months, and depression. These effects on the central nervous system will likely disappear within the first few days of folate supplementation (5, 6).
Pregnancy Complications
Maternal folate deficiency may cause spontaneous abortion, preterm birth, placental abruption, congenital disorders such as neural tube defects, and severe language delay in children. Folate deficiency during pregnancy can also cause autism spectrum disorder development in the child (5).
Other Symptoms
Other folate deficiency symptoms include mouth soreness, ulcerations on the tongue and mouth, pigmentation changes in skin, hair, or fingernails, anorexia, weight loss, and gastrointestinal symptoms such as nausea, vomiting, cramps, and diarrhea (6).
Oral ulcers might appear alone, without neurological symptoms of folate deficiency, as opposed to vitamin B12 deficiency (7).
Folate & Human Health
Autism Spectrum Disorder (ASD)
Evidence suggests that folacin use before and after conception might decrease the risk of ASD development in the child, probably due to folate’s role in methylation processes affecting the development of the nervous system.
Several observational studies have found associations between maternal folic acid or multivitamin use before and during pregnancy and a lower risk of ASD. The Norwegian Mother and Child Cohort Study (NMCCS), including over 85,000 children from ages 3 to 10, found that mothers taking up to 400 mcg of folic acid daily during pregnancy or starting to 4 weeks prior and 8 weeks after conception were 39% less likely to have children with ASD.
A US population-based study of 837 children found that children born to mothers consuming 600 mcg or more of folic acid daily during the first 4 weeks of pregnancy had a 38% lower risk of ASD. A similar study of over 45,300 Israeli children also linked folic acid or multivitamin intake before or during pregnancy to a decreased risk of ASD in their offspring. In contrast, a Danish cohort study of over 35,000 pregnant women and their children showed no relation between periconceptional folacin or multivitamin supplementation and ASD (1).
Periconceptional folic acid use might decrease the increased risk of ASD in children exposed to antiepileptic drugs during their intrauterine life. The analyzed data from NMCCS, including nearly 105,000 children, found that those exposed to antiepileptic drugs were 6 to 8 times more likely to have autistic traits if their mothers did not take folic acid than if they did (1).
Supplementing with moderate amounts of folic acid and vitamin B12 might reduce the risk of ASD in offspring, whereas excessive folate and vitamin B12 levels during pregnancy may significantly increase it. During a briefing, Margaret Daniele Fallin, PhD, stated, "So for now, the public health message is, supplementation is good, but there may be a subset of women whose levels are extremely high, and these extreme levels may be harmful" (8).
Cognitive Function & Dementia
Many studies have found associations between low serum folate concentrations and elevated homocysteine levels and Alzheimer’s disease and dementia. According to the current hypothesis, elevated homocysteine levels might increase dementia risks due to brain ischemia (leading to neuronal cell death), tangle deposition, and the inhibition of methylation reactions. However, folic acid supplementation has not been shown to affect cognitive function or the risk of developing dementia or Alzheimer’s (1).
In several clinical trials, folic acid supplementation alone or with other vitamins has lowered serum homocysteine levels but did not improve cognitive performance in people with or without cognitive impairment. Moreover, a meta-analysis of 11 randomized trials of more than 20,000 adults aged 60-82 found that supplementing folic acid with vitamin B12 lowered homocysteine levels but did not affect global cognitive function or specific domains such as memory, speed, and executive function (1, 9).
Interestingly, one trial favored folic acid supplementation; 818 participants aged 50-70 took folic acid supplementations daily and had improved global cognitive function, memory, and information processing speed. An Australian study analysis found that intake of 400 mcg of folic acid with 100 mcg of vitamin B12 daily improved some measures of cognitive performance, mainly memory, in 900 adults aged 60-74 with depression (1, 10).
Depression
Studies found a link between low folate levels and poor response to antidepressant therapy (1, 10).
A study of around 2,900 people aged 15-39 in the US noted that those with major depression had significantly lower folate serum and erythrocyte (red blood cell) concentrations than those who had not been depressed (1).
A 2005-2006 NHANES data analysis found that higher folate serum concentrations were associated with a lower depression prevalence in almost 2,800 adults, predominantly women.
Studies had mixed results regarding folic acid intake as an addition to antidepressant medications. A clinical trial of 127 patients with major depression assigned 500 mcg of folic acid in addition to fluoxetine showed significant improvement in depressive symptoms in women but not men. However, a meta-analysis of similar clinical trials demonstrated no improvement in depression symptoms and folic acid intake.
5-MTHF (active form of vitamin B9) might be a better option as an adjuvant treatment to SSRI antidepressants than folic acid. Based on low-quality evidence, some scientists noted that a 15,000 mcg daily intake of 5-MTHF combined with fluoxetine or other antidepressants might be effective in depression treatment.
The British Association for Psychopharmacology and the Canadian Network for Mood and Anxiety Treatment Guidelines also stated that 5-MTHF might be an effective addition to SSRI antidepressants for treating depressive disorders (1, 11, 12).
Neural Tube Defects
Neural tube defects, or NTDs, lead to spinal cord defects (spina bifida) and anencephaly, the absence of some parts of the skull and brain. The prevalence rate of these NTDs is 5.5 to 6.5 per 10,000 births in the US. Hispanic women have the highest rates, whereas non-Hispanic black women have the lowest rates (1).
Additionally, the 677C>T MTHFR polymorphism is more common in Hispanics compared to Caucasians, Asians, and African Americans.
The Food and Nutrition Board, US Public Health Service, and the CDC recommend consuming 400 mcg of folic acid daily from supplements, enriched foods, or both to help prevent NTDs, even in those with 677C>T MTHFR polymorphism (1, 3, 13).
The U.S. Preventive Services Task Force (USPSTF) suggests taking 400-800 mcg of folic acid daily for at least one month before conception and during the first two to three months of pregnancy. People at risk of folate deficiency should counsel a physician to adjust folic acid doses (1, 14, 15).
Preterm Birth & Congenital Disorders
Observational studies noted that folic acid supplementation might lower the risk of preterm birth. Supplementation several months before conception might decrease the risk by up to 50-70% (1, 16).
Heart tissue cells require large amounts of folate to develop properly; thus, folic acid supplementation with multivitamins might minimize the risk of congenital heart defects. Infants and children with congenital heart defects often show impaired folate metabolism, with low folate or vitamin B12 levels and elevated homocysteine levels in the blood (17).
A large population-based cohort study in Canada from 1990 to 2011 concluded that adding folic acid to foods (fortifying foods) reduced the rate of non-genetic congenital heart defects by 11%. Another population-based study in Atlanta noted that women who took multivitamins containing folic acid during the periconceptional period reduced the risk of congenital heart defects by 24% (1).
Studies have also linked folic acid intake combined with multivitamin supplements to a reduced occurrence of urinary tract anomalies at birth, oral facial clefts, limb defects, and hydrocephalus, a condition characterized by excess cerebrospinal fluid (CSF) buildup within parts of the brain (1).
Cardiovascular Disease & Stroke
As mentioned in the “Folate Deficiency” section, elevated homocysteine due to folate or vitamin B12 deficiency has been linked to heart disease.
Folic acid and vitamin B12 supplementation lowers homocysteine levels and might protect against stroke but not decrease the risk of heart disease. In a study of 5,442 US women aged 41 or above, at high risk of heart disease, daily folic acid and vitamins B6 and B12 supplementation for over 7 years did not reduce the risk of major cardiovascular events, nor did it affect the biomarkers of vascular inflammation. Another similar study, including people aged 55 years or older with vascular disease or diabetes, came to the same conclusion (1).
According to current evidence, folic acid supplementation alone or combined with vitamins B6 and B12 does not reduce the risk of heart disease. Still, it reduces the risk of stroke, especially in areas with low folate intake (1, 18, 19).
In a large Chinese trial, folic acid with 10 mg enalapril (used to treat high blood pressure) significantly reduced the risk of stroke by 21% compared to enalapril alone. An analysis of this trial found that those with low platelet count and elevated homocysteine levels had a 73% decreased risk of stroke after folic acid supplementation compared to those with high platelet count (1).
Cancer
Several epidemiological studies have demonstrated an inverse association between folate intake and folate status and the risk of several cancers: colorectal, lung, cervical, ovarian, breast, bladder, esophageal, stomach, pancreatic, and others. The exact mechanism has not been established, but it is suggested to be due to folate’s role in DNA replication and cell division. However, the results of several clinical trials demonstrated that folic acid intake might increase the risk of cancer or have no effect on overall cancer incidence (1).
Folate might play a dual role in cancer risks: it might suppress some types of early-stage cancers, while its high doses consumed after the paraneoplastic lesions might promote cancer development and progression (1, 3, 20, 21).
A trial in France included 2,501 people with a history of heart disease who took folic acid, vitamins B6, and B12 daily for 5 years and found no associations between B-vitamin intake and cancer outcomes. In contrast, two similar trials in Norway, which lasted 39 months, found a significant increase in cancer risks and vitamin B supplementation (1).
A thorough research has focused on folate’s role in colorectal adenoma and cancer risks. The NIH-AARP Diet and Health Study of over 525,000 people aged 50-71 in the US demonstrated that individuals taking 900 mcg daily folate had a 30% lower cancer risk than those taking less than 200 mcg daily. However, studies like Women’s Antioxidant and Folic Acid Cardiovascular Study and three large clinical trials (in Canada, the US, the UK, and Denmark) have found no significant associations (1).
A meta-analysis of 13 trials found no statistically significant effect of folic acid intake over 5 years on the risk of colorectal, lung, breast, prostate, or other cancers. In contrast, some research has shown an increased risk of gastrointestinal and prostate cancers in those supplementing with folic acid. Similarly, another study found that folic acid intake from enriched foods and supplements was associated with an increased risk of cancer recurrence with bladder cancer. Higher plasma folate levels have also been linked to an increased risk of breast cancer in those with BRCA1 or BRCA2 mutation (1).
Overall, more research is needed to understand better the effects of dietary and supplemental folate on cancer risks and how their effects differ depending on the timing of exposure.
Folate Toxicity & Vitamin B12 Anemia
As previously mentioned, both folate and vitamin B12 deficiency may lead to megaloblastic anemia. Large amounts of folate intake might mask vitamin B12 deficiency, which can lead to irreversible neurological consequences in some cases. On the other hand, folate intake might precipitate or exacerbate symptoms of anemia and cognitive impairment in those with B12 deficiency. Thus, vitamin B12 deficiency must be ruled out before folic acid intake (7).
Intake of large amounts of folic acid may exceed the body’s ability to convert folate, leading to unmetabolized folic acid and subsequent impaired immune response and cognition among older adults (1).
The table below shows the tolerable upper intake limits of vitamin B9 from supplements or food sources. These values do not apply to individuals taking high folate doses under medical supervision.
| 1-3 years | 4-8 years | 9-13 years | 14-18 years | 19+ |
| 300 mcg | 400 mcg | 600 mcg | 800 mcg | 1000 mcg |
The tolerable upper intake limit is the same during pregnancy and lactation (1).
Folate Contraindications & Interactions
Folate is contraindicated in patients with a previous allergic reaction to folic acid supplements.
Folic acid supplements interact with methotrexate, antiepileptic medications, barbiturates, and sulfasalazine. Antibiotics, zinc-containing lozenges, and cholestyramine might also interfere with folate absorption (1, 22).
Methotrexate (Rheumatrex, Trexall) is used to treat cancer, psoriasis, inflammatory bowel disease, rheumatoid arthritis, and other autoimmune conditions. It is an antagonist to folate, and folic acid might interfere with methotrexate’s anticancer effects (1).
Antiepileptic medications, such as phenytoin (Dilantin), carbamazepine (Carbatrol, Tegretol, Equetro, Epitol), valproate (Depacon), and barbiturates, might reduce serum folate levels. Up to 90% of patients may have reduced folate levels (1, 23).
Sulfasalazine (Azulfidine) is a first-line medication for ulcerative colitis. It blocks the intestinal absorption of folate and might cause folate deficiency (1).
Caffeine, green, and oolong teas contain high catechin levels, which might block folic acid absorption. However, several studies failed to find an association between caffeinated beverage intake and folate deficiency risk (24, 25).
Summary
Folate is the naturally occurring vitamin B9, whereas folic acid is the synthetic form of the vitamin used in dietary supplements and enriched or fortified foods (e.g., rice, pasta, bread, and breakfast cereals).
Folic acid is commonly used to manage megaloblastic anemia and decrease the risk of neural tube defects (NTD).
Compared to folate, folic acid is more stable to heat; thus, less folic acid is lost during cooking, making it more suitable for adding to foods.
Folate is naturally found in vegetables, primarily dark leafy greens and legumes, fruits and fruit juices, nuts, seafood, eggs, dairy products, red meat, and poultry. It can also be added to foods, as written on the packaging.
Folate deficiency may result from inadequate diets, diseases affecting folate absorption or metabolism, several genetic disorders and medicines, alcoholism, malignancy, pregnancy, lactation, MTHFR genetic polymorphism 677C>T, hemolytic anemia, dialysis, and vitamin B12 and zinc deficiencies.
Folate deficiency results in anemia, pregnancy complications, and neurological and gastrointestinal symptoms.
Folic acid supplements interact with methotrexate, antiepileptic medications, barbiturates, and sulfasalazine.
References
- https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
- https://medlineplus.gov/ency/article/002408.htm
- https://www.cdc.gov/ncbddd/folicacid/faqs/faqs-general-info.html
- https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- https://emedicine.medscape.com/article/200184-overview
- https://emedicine.medscape.com/article/200184-overview
- https://www.ncbi.nlm.nih.gov/books/NBK554487/
- https://www.medscape.com/viewarticle/863216
- https://academic.oup.com/ijnp/article/25/2/136/6428560#332797039
- https://www.frontiersin.org/articles/10.3389/fnagi.2022.966933/full
- https://www.bap.org.uk/pdfs/BAP_Guidelines-Antidepressants.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4994794/
- https://www.bscc.ca.gov/wp-content/uploads/2011-DRI-of-the-Food-and-Nutrition-Board.pdf
- https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/folic-acid-for-the-prevention-of-neural-tube-defects-preventive-medication
- https://www.medscape.com/viewarticle/995061
- https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000061
- https://cdt.amegroups.org/article/view/24182/
- https://svn.bmj.com/content/3/2/51
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5836580/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9287768/
- https://journals.sagepub.com/doi/10.1177/03000605231223064
- https://www.nhs.uk/medicines/folic-acid/taking-folic-acid-with-other-medicines-and-herbal-supplements/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC320966/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6143377/
- https://reference.medscape.com/drug/folvite-folic-acid-344419