Phosphorus — Rich Foods, Deficiency, Recommended Intakes, and Benefits
Introduction
Phosphorus (P) is an essential mineral found mainly in the bones and teeth. It is required for the regulation of gene transcription, activation of various enzymes, maintenance of normal pH in extracellular fluid (fluid outside of the cells), and energy storage in the cells (1).
Содержание
- Absorption, Metabolism, & Regulation
- Physiological Functions & Health Benefits
- Recommended Intakes
- Phosphorus Rich Foods
- Effects of Phosphorus on the Human Body
- Phosphorus Deficiency or Hypophosphatemia
- Phosphorus Toxicity or Hyperphosphatemia
- Supplements & Contraindications
- Interactions With Medications
- Summary
- References
Phosphorus vs Phosphate
Sometimes, the terms are used interchangeably, but they are not the same. In the organism, elemental phosphorus (P) is part of other organic and inorganic compounds, such as phosphates (H2 PO4 - and HPO42-) (2).
Around 85% of phosphates are in inorganic forms in our skeleton, whereas around 15% are present as organic compounds (phosphoproteins, phospholipids, and nucleic acids) in the soft tissues and blood (1, 3).
Absorption, Metabolism, & Regulation
Most dietary phosphorus is in the form of phosphates and phosphate esters; however, in seeds and unleavened bread, it is in the form of phytic acid. Phytic acid is considered the storage form of the mineral and is unavailable for absorption due to the lack of phytase enzymes (1).
About 60 to 80% of phosphorus undergoes passive absorption in the small intestines, whereas the rest is absorbed by active transport.
Phosphorus is interrelated with calcium, as hormones such as vitamin D and parathyroid hormone (PTH) regulate the metabolism and control the levels of both minerals. These two minerals—calcium and phosphorus—make up hydroxyapatite (Ca5(PO4)3(OH)), the main structural component of tooth enamel and bones, which provides hardness.
Other hormones, such as estrogen and adrenaline, also affect phosphorus metabolism and homeostasis. For example, people on estrogen therapy tend to have lower serum phosphorus levels and increased urinary excretion rates (1, 4). Patients with chronic kidney failure tend to have increased serum phosphate levels as the body cannot efficiently excrete phosphate.
In healthy individuals, the kidneys, bones, and intestines regulate phosphorus homeostasis by balancing urinary excretion with intestinal absorption, regulating fibroblast growth factor (FGF23), and ensuring phosphorus’s adequate deposition and resorption from bones (1).
Fibroblast growth factor is another hormone produced in the bones that increases phosphate excretion through the kidneys.
Physiological Functions & Health Benefits
In this section, we’ll look into phosphorus’s physiological functions and benefits (1, 2, 5, 6, 7):
- Phosphate is one of the main components required for bone mineralization and endochondral ossification. Bone mineralization begins in the matrix vesicles (structures located at sites of initial calcification in bones, cartilage, and predentin), where hydroxyapatite is formed. Endochondral ossification of the bone happens due to increased phosphate levels within the cells, where phosphate induces the death of terminally differentiated chondrocytes for further mineral deposition and bone formation.
- Phosphate is required for the mineralization of the structural components of the teeth: enamel, dentin, cementum, and alveolar bone.
- Phosphate is an essential component of cell membranes, DNA, RNA, and proteins and is required for several enzymatic reactions, such as the breakdown of glucose for energy production and the formation of ammonia. Additionally, phosphate is required to convert ADP (adenosine diphosphate) to ATP (adenosine triphosphate), the cell’s energy currency, required for the transport of ions, muscle contraction, nerve impulse propagation, phosphorylation of substrates, and synthesis of various molecules.
- Phosphate is also a building block for creatine phosphate and the coenzyme NADP, and phospholipids.
- Phosphate regulates the oxygen-carrying capacity of hemoglobin.
- Inorganic phosphate (HPO42-) acts as a urinary buffer, and it can reversibly bind with free hydrogen ions (H+). When the fluid is resorbed within the kidney tubules, the concentration of phosphate increases, making it an excellent buffer.
Recommended Intakes
According to the 2020-2025 Dietary Guidelines for Americans, the recommended dietary allowance (RDA) of phosphorus for adults is 700mg.
The table below shows the changes in the RDA of phosphorus based on age. The Food and Nutrition Board established an adequate intake equivalent to what is consumed by healthy, breastfed infants from birth to 12 months (1, 8).
| Up to 6 months | 7-12 months | 2-3 years | 4-8 years | 9-18 years | 19+ years |
| 100mg | 275mg | 460mg | 500mg | 1250mg | 700mg |
The RDA values don’t change during pregnancy and lactation.
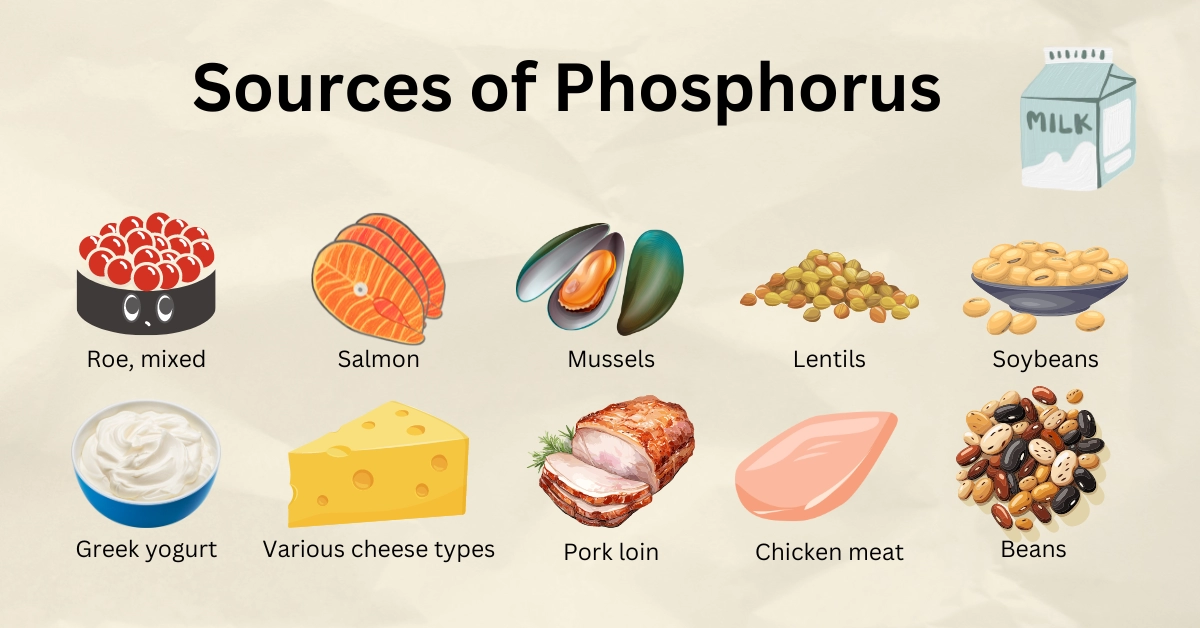
Phosphorus Rich Foods
Many types of foods contain phosphorus: dairy products, eggs, meat, poultry, fish, vegetables, legumes, nuts, and whole grains. In the US, dairy products provide around 20% of the recommended amount of phosphorus, and bakery products about 10%.
The absorption rate of phosphorus ranges from 40 to 70%. Phosphorus derived from an animal source has a higher absorption rate than that from plants. Additionally, dietary and supplementary calcium can bind to phosphorus, decreasing its absorption rate.
The table below shows foods rich in phosphorus and its levels per 1 serving.
| Roe, mixed species, cooked | 438mg in 3oz (85g) |
| Yogurt, Greek, plain | 230mg in 1 container (170g) |
| Milk | 232mg in 1 cup (244g) |
| Salmon, chinook, cooked | 315mg in 3oz |
| Salmon, sockeye, cooked | 259mg in 3oz |
| Mussels, blue, cooked | 242mg in 3oz |
| Cottage cheese | 180mg in 4oz (118g) |
| Mozzarella | 692mg in 1 cup (132g) |
| Chicken meat, cooked | 155g in 3oz |
| Pork, loin, cooked | 209mg in 3oz |
| Lentils, cooked | 356mg in 1 cup (198g) |
| Soybeans, mature, cooked | 421mg in 1 cup (172g) |
| Cashew | 168mg in 1oz (28.35g) |
| Almond | 136mg in 1oz |
| Potatoes, cooked | 104mg in 1 NLEA serving (148g) |
| Kidney beans, cooked | 244mg in 1 cup (177g) |
| Black turtle beans, cooked | 281mg in 1 cup (185g) |
| Rice, long-grain, cooked | 67.9mg in 1 cup (158g) |
| Peas, cooked | 187mg in 1 cup (160g) |
| Egg, hard-boiled | 86mg in 1 large egg (50g) |
Phosphate additives (absorption rate of 70%) such as phosphoric acid and sodium phosphate are present in many foods and are estimated to provide 10-50% of total phosphorus intake in Western countries. Phosphate additives can be found in sausage, bacon, baked goods, soft drinks, energy drinks, instant noodles and rice, frozen meals, frozen or canned fish, and more.
Effects of Phosphorus on the Human Body
Chronic Kidney Disease
Chronic kidney disease (CKD) affects up to 10% of the population, causing kidney function decline and leading to less efficient phosphate excretion and, thus, to serum phosphate level elevations (positive phosphate balance). Due to this, parathyroid hormone and FGF23 become unable to suppress phosphorus reabsorption by the kidneys (1).
Increased phosphorus levels may lead to bone disorder and calcification of the blood vessels and soft tissues. Chronic kidney disease, accompanied by bone disease, leads to elevated phosphate concentrations in the blood. The excess accumulates in soft tissue organs and blood vessels (9).
According to studies, CKD and elevated serum phosphate are risk factors for kidney and heart disease progression and mortality in general (10). A meta-analysis including 199,289 middle-aged patients with end-stage kidney disease showed that dialysis patients with the highest phosphate levels had a 39% greater risk of mortality than those with normal levels of phosphate. However, high phosphate concentrations are less likely to have the same effects in those with mild chronic kidney disease (1)
Clinicians sometimes advise patients to limit their phosphorus intake by replacing animal-based proteins with plant-based ones, as the latter’s phosphorus is less bioavailable, and consuming more foods rich in calcium in order to decrease the risk of disease complications.
Interestingly, a Cochrane review including 634 patients with kidney disease followed for 1-18 months demonstrated the evidence indicating that dietary changes might positively impact chronic kidney disease is limited and low-quality (1).
A clinical practice guideline for chronic kidney disease and mineral and bone disorder recommends that patients with more severe (stage 3-5) kidney disease limit their phosphorus intake. Extreme dietary restriction of phosphorus is not suggested, as it can cause physical (malnutrition) and mental functional impairments (1, 11).
Cardiovascular Disease
Several observational studies noted that high serum phosphate levels are consistently associated with heart failure, cardiovascular disease risk in people with or without a history of heart disease, and the risk of all-cause mortality (1,12, 13).
An analysis of over 14,000 individuals without atrial fibrillation (a type of arrhythmia) on almost 20 years of follow-up found that each 1mg/dL increase in serum phosphate levels increased the risk of atrial fibrillation by 13%.
Chronic kidney disease and high dietary phosphate intake may elevate FGF23 levels, increasing the risk of not only atrial fibrillation but also left ventricular hypertrophy, congestive heart failure, and mortality. Moreover, high phosphate concentrations damage the endothelial cells (the inner lining of blood vessels) and vascular smooth muscle cells (14).
A meta-analysis including 13,515 individuals (over 50% men) followed for 6 to 29 years showed those with the highest phosphate levels (2.79–4.0 mg/dL) had a 36% increased risk of cardiovascular mortality. A subsequent study of 13,165 individuals (52% women) followed for 14 years found that each 1mg/dL increase in serum phosphate levels above 3.5mg/dL increased the overall death risk by 35% and cardiovascular death risk by 45%.
However, not all data supports a link between serum phosphate levels and heart disease risk. For example, data analysis from 7,269 postmenopausal women with osteoporosis found no associations during 4 years of follow-up (1).
Cancer
High amounts of dietary phosphorus in the Western diet are considered a risk factor for cancer formation. A case-control study has measured risk ratios of dietary phosphorus levels linked to self-reported breast cancer in women of middle age. Results have found that the highest phosphorus intake was associated with a clinically significant risk of breast cancer incidence compared to the recommended dietary levels for the treatment of chronic kidney disease (15).
Bone Health
Inorganic phosphate induces programmed cell death of overgrown chondrocytes. Low phosphate levels reduce hydroxyapatite levels and impair programmed cell death, leading to rickets or osteomalacia (16, 17).
On the other hand, diets high in phosphorus are not always safe either. High phosphorus and low calcium intakes may lead to reduced serum calcium levels, stimulating PTH. Increased PTH releases the calcium from the bones to keep in homeostatic concentrations, leading to decreased bone mineral density.
In animal models, high dietary phosphorus has been shown to decrease bone density or cause bone loss. Moreover, for every 100mg of dietary phosphorus, the fracture risk increased by 9%.
Cola beverages contain phosphoric acid, which has been shown to decrease calcium absorption, while the majority of other carbonated soft drinks do not contain phosphoric acid (18).
Phosphorus Deficiency or Hypophosphatemia
Hypophosphatemia is rare in the US, almost never results from low dietary phosphorus intake, and is relatively frequent among inpatients.
Hypophosphatemia symptoms include anorexia, anemia, muscle weakness, impaired immunity, paresthesia (feeling of tingling, burning, itching, or numbness), uncoordinated movements, confusion, and bone problems such as bone pain, rickets, and osteomalacia. In severe cases, low phosphate levels can lead to stupor, coma, and even death.
Hypophosphatemia may be chronic and acute due to various reasons (1, 2, 19, 20):
- Primary or secondary hyperparathyroidism (high PTH levels in the blood)
- Kidney tubule defects or damage, Fanconi syndrome, long-term use of diuretics
- Familial hypophosphatemia
- Chronic diarrhea, malabsorption (impaired absorption of nutrients)
- Post-insulin administration, diabetic ketoacidosis, respiratory alkalosis,
- Glucose administration, corticosteroid medications
- Refeeding syndrome (people with severe malnutrition may develop this syndrome after several days of starting enteral or parenteral nutrition due to metabolism shift; magnesium, potassium, thiamine, and other nutrients may also be decreased)
- Severe alcohol use disorder
- Severe burns
- Acute diarrhea and vomiting
- Long-term intake of antacids and theophylline.
Phosphorus Toxicity or Hyperphosphatemia
High dietary phosphorus rarely leads to adverse effects in healthy people; however, as discussed above, some studies have found associations between high dietary phosphorus intake and the risk of cardiovascular, kidney, and bone disease and an increased risk of death, whereas others found no such associations.
Rapid elevation of serum phosphate levels causes calcium to combine with phosphate, causing hypocalcemia (low blood calcium), which manifests with tetany, seizures, and decreased blood pressure. Chronic hyperphosphatemia is linked to soft-tissue calcification.
The most common cause of hyperphosphatemia is chronic kidney disease with impaired kidney function; other less common causes include (2, 21):
- Acute kidney disease, kidney tubular resorption
- Hypoparathyroidism (low PTH levels in the blood)
- Pseudohypoparathyroidism (lack of response to normal PTH levels)
- Diabetic ketoacidosis or lactic acidosis
- Acromegaly
- Crush injuries
- Sepsis
- Cell lysis or destruction, such as rhabdomyolysis (destruction of muscle tissue), intravascular hemolysis, leukemia, lymphoma, and therapy with cytotoxic agents.
- Increase phosphate intake, such as phosphate-containing laxatives
Tolerable upper limit (UL) intakes have been developed for dietary phosphorus intake, which does not apply to those taking phosphorus medications under medical supervision (1).
| 1-8 years | 9-13 years | 14-50 years | 51-70 years | 71+ years | |
| Male/ Female | 3000mg | 4000mg | 4000mg | 4000mg | 3000mg |
| Pregnancy | - | - | 3500mg | - | - |
| Lactation | - | - | 4000mg | - | - |
Supplements & Contraindications
Dietary supplements containing phosphorus come in many forms: those containing only phosphorus and those containing other ingredients, minerals, and vitamins.
Most phosphorus supplements are in the form of phosphate salts (has approximately 70% bioavailability), such as dipotassium phosphate or disodium phosphate, and phospholipids, such as phosphatidylcholine or phosphatidylserine (1).
Phosphorus-containing pills are contraindicated for people with previous allergic reactions to one or more of the components, people with infected phosphate stones in the urinary tract, people with impaired kidney function, and hyperphosphatemia (22).
Interactions With Medications
- Long-term use of antacids containing aluminum hydroxide (Maalox HRF and Rulox). They bind to phosphorus in the intestines and decrease its absorption. Use of antacids for 3 months or longer may lead to decreased serum phosphorus levels.
- Some laxatives (such as Fleet Prep Kit #1) contain sodium phosphate, which may increase serum phosphate levels. According to the FDA, these products may be potentially dangerous if used in more than recommended doses, especially in people with kidney or heart disease or dehydration (1).
- Theophylline (used to treat asthma) may have a distinct biological effect on kidney tubular activity and increase the excretion of phosphorus and calcium (23).
Summary
Phosphorus (P) is an essential mineral found in large amounts in our bones and teeth. It is required for the regulation of gene transcription, activation of various enzymes, maintenance of normal pH in extracellular fluid (fluid outside of the cells), and energy storage in the cells.
Phosphorus is interrelated with calcium, as hormones such as vitamin D and parathyroid hormone (PTH) regulate the metabolism and control the levels of both minerals. In healthy individuals, phosphorus homeostasis is regulated by the kidneys, bones, and intestines.
According to the 2020-2025 Dietary Guidelines for Americans, the RDA of phosphorus for adults is 700mg.
Many foods contain phosphorus: dairy products, eggs, meat, poultry, fish, vegetables, legumes, nuts, and whole grains. Phosphorus derived from an animal source has a higher absorption rate than that from plants.
Chronic kidney disease causes kidney function to decline, leading to less efficient phosphate excretion and elevated serum phosphate levels. Increased phosphorus levels may lead to decreased bone density and calcification of the blood vessels and soft tissues.
Long-term use of antacids containing aluminum hydroxide may lead to decreased phosphate levels in the blood, whereas long-term use of several laxatives containing sodium phosphate may lead to increased phosphate concentrations.
References
- https://ods.od.nih.gov/factsheets/Phosphorus-HealthProfessional/
- https://emedicine.medscape.com/article/2090666-overview#showall
- https://www.ncbi.nlm.nih.gov/books/NBK279023/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3849680/
- https://www.ncbi.nlm.nih.gov/books/NBK560925/
- https://www.jci.org/articles/view/34174
- https://www.ncbi.nlm.nih.gov/books/NBK553175/
- https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3139680/
- https://www.nature.com/articles/nrneph.2016.164
- https://www.mdpi.com/2072-6643/13/5/1670
- https://www.ahajournals.org/doi/10.1161/ATVBAHA.123.319198#
- https://www.ahajournals.org/doi/10.1161/circulationaha.105.553198
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5911324/
- https://www.mdpi.com/2072-6643/15/17/3735
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461213/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6443631/
- https://academic.oup.com/nutritionreviews/article/70/6/311/1846932
- https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/hypophosphatemia-low-level-of-phosphate-in-the-blood
- https://www.ncbi.nlm.nih.gov/books/NBK564513
- https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/hyperphosphatemia-high-level-of-phosphate-in-the-blood
- https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=60387fe2-bbc1-4b19-866f-1456adbc1096&type=display
- https://pubmed.ncbi.nlm.nih.gov/6095002/
